OCD Awareness: Seeing the Disorder Clearly
There’s a big difference between enjoying a tidy space and living with obsessive-compulsive disorder, and confusing the two can be more harmful than we realize. Being neat is a preference; OCD is a mental health condition driven by anxiety, intrusive thoughts, and a desperate need to relieve anxiety and distress. Someone who likes things organized might feel satisfied after straightening their desk, but a person with OCD may rearrange those same items repeatedly, not out of enjoyment, but out of fear that something terrible will happen if they don’t. When we casually say “I’m so OCD” to describe being particular or organized, we minimize the very real struggle of those battling relentless mental compulsions. Understanding the difference isn’t just about using the right language. It’s about acknowledging the lived experiences of those who are truly affected.
Did you know that 1 in 40 adults struggle with OCD at some point in their lives? That’s millions of people, almost enough people to fill New York City! And that number doesn’t include children and teens, even though OCD can show up at any age.
OCD is one of the most misunderstood mental health conditions out there. It’s often portrayed as quirky habits or perfectionism, but in reality, it’s exhausting, intrusive, and anything but a personality trait.
If you’re dealing with constant mental loops, compulsions you have to follow, or fears you can’t explain to anyone without feeling “crazy,” you’re not alone. And no, you’re not broken. You’re dealing with OCD.
What Obsessive-Compulsive Disorder Is
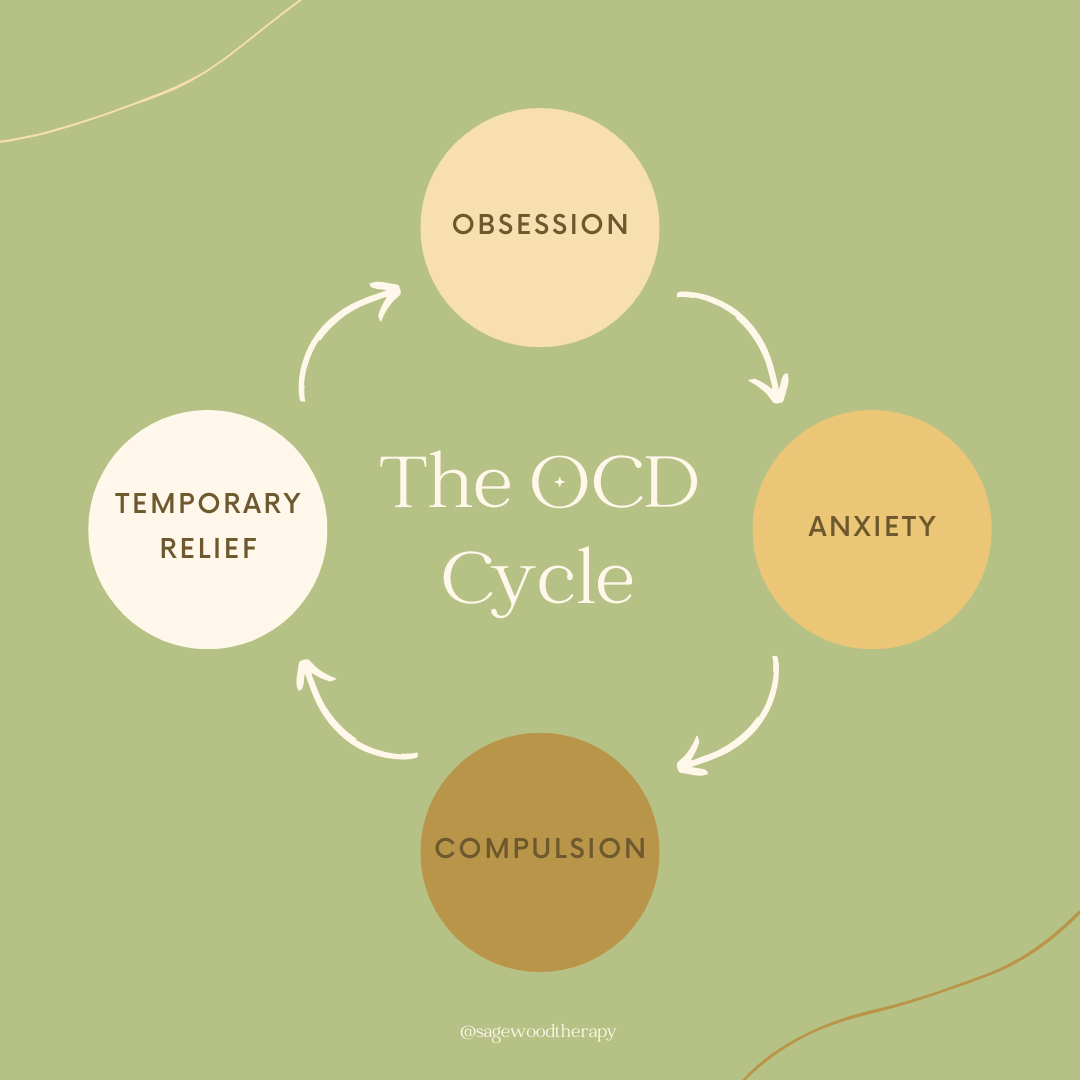
OCD involves two key parts: Obsessions are unwanted, intrusive thoughts, fears, or images that create anxiety, compulsions are behaviors (physical or mental) you do to relieve that anxiety.
Obsessions can have various triggers depending on the type of OCD, and many people can experience obsessions. Someone with ordering and arranging OCD may have obsessions that convince them that something terrible can happen to them or their loved ones if they don’t rearrange items in a specific way. “If this isn’t in order, something bad is going to happen,” or “this doesn’t feel right and I can’t relax until it’s fixed” may be common obsessions that come to mind that cause intense distress. The person may then rearrange things in a specific order multiple times until they feel relief from the anxiety, also known as the compulsion.
The purpose of a compulsion is to alleviate the anxiety and distress associated with the obsession. It sounds like these behaviors should be okay because they help us calm down from a thought that’s so silly and unrealistic, right? But anxiety can actually thrive from those actions because the compulsions reinforce the belief that the obsessions are true. The more someone with OCD engages in compulsions, the more their obsessions and anxiety can grow. This becomes the vicious cycle of OCD.
It’s not something you choose. You don’t want to do the compulsions, but you just feel like you have to. And if you don’t, something bad will happen.
Common Types of OCD
Contamination & Cleaning OCD – Fear of germs, illness, or environmental hazards, often leading to excessive washing or avoidance.
“If I get sick, I’ll get my family sick, and then they will die.”
Checking – Repeatedly checking locks, appliances, or actions to prevent something bad from happening.
“Did I turn the stove off? What if the house is burning down?”
Harm OCD — Intrusive fears of unintentionally or intentionally harming oneself or others.
“I hit a bump in the road while driving, what if I accidentally ran someone over? I have to check.”
Religious/Moral Scrupulosity – Excessive guilt or fear of moral or spiritual wrongdoing.
“That prayer didn’t feel right, I should say it again or I might go to hell.”
Sexual or Identity-Based OCD — Unwanted, intrusive thoughts about sexuality or identity that do not reflect your true identity.
“What if I’m attracted to the same-sex?”
“Just Right” OCD — A need for things to feel perfect, aligned, or symmetrical. Not for aesthetics, but to relieve internal discomfort.
“This is out of place, I have to fix it until it’s right.”
Relationship OCD — Persistent fears or doubt about the quality of the relationship. May focus on flaws, compare the relationship and/or partner to others, and need constant reassurance.
“I was attracted to another person. Am I not faithful to my partner?”
If none of these fit perfectly, it doesn’t mean it’s not OCD. OCD comes in countless variations and each person’s OCD is unique to them. Therefore, treatment for OCD may look different for everyone.
OCD Sounds Complicated… How is it treated?
There are several effective treatments that can help manage OCD, including medication and therapies such as Acceptance and Commitment Therapy (ACT), Inference-Based Cognitive Therapy (I-CBT), mindfulness-based approaches, and Dialectical Behavior Therapy (DBT). However, it’s essential to work with a therapist who specializes in OCD, because some well-intentioned strategies can accidentally make symptoms worse. For example, coping skills that are used to reduce anxiety in the moment can sometimes become new compulsions, which keeps the OCD cycle going.
That’s why the gold-standard treatment for OCD is Exposure and Response Prevention (ERP), a targeted approach designed specifically to break that cycle rather than reinforce it.
Exposure and Response Prevention
Exposure and Response Prevention is a type of cognitive-behavioral therapy (CBT), and a structured therapy method that helps retrain your brain to stop reacting to intrusive thoughts with compulsions. ERP usually begins with the therapist providing education on OCD and thoroughly assessing the patterns of obsessions and compulsions. After gathering more information about the OCD, you and your therapist will work together to create a hierarchy of thoughts, triggers, or situations that activate the obsession and fear. This serves as your list of exposures to the obsessions your therapist will help you gradually confront either in real life, or through imaginal exercises. By facing these fears through exposure, we teach our brain that the anxiety will go down on its own without the compulsion, and we learn the scary outcomes we feared don’t happen.
If OCD has taken over your time, your peace, or your sense of self — it doesn’t have to stay that way. Support is available, and real change is possible. As a trained ERP therapist, my goal is to work collaboratively with you to help you take your life back from OCD. Contact me today to schedule a consultation!